National Healthcare Reform Unveiled: Trump Administration Proposes $200 Billion Plan
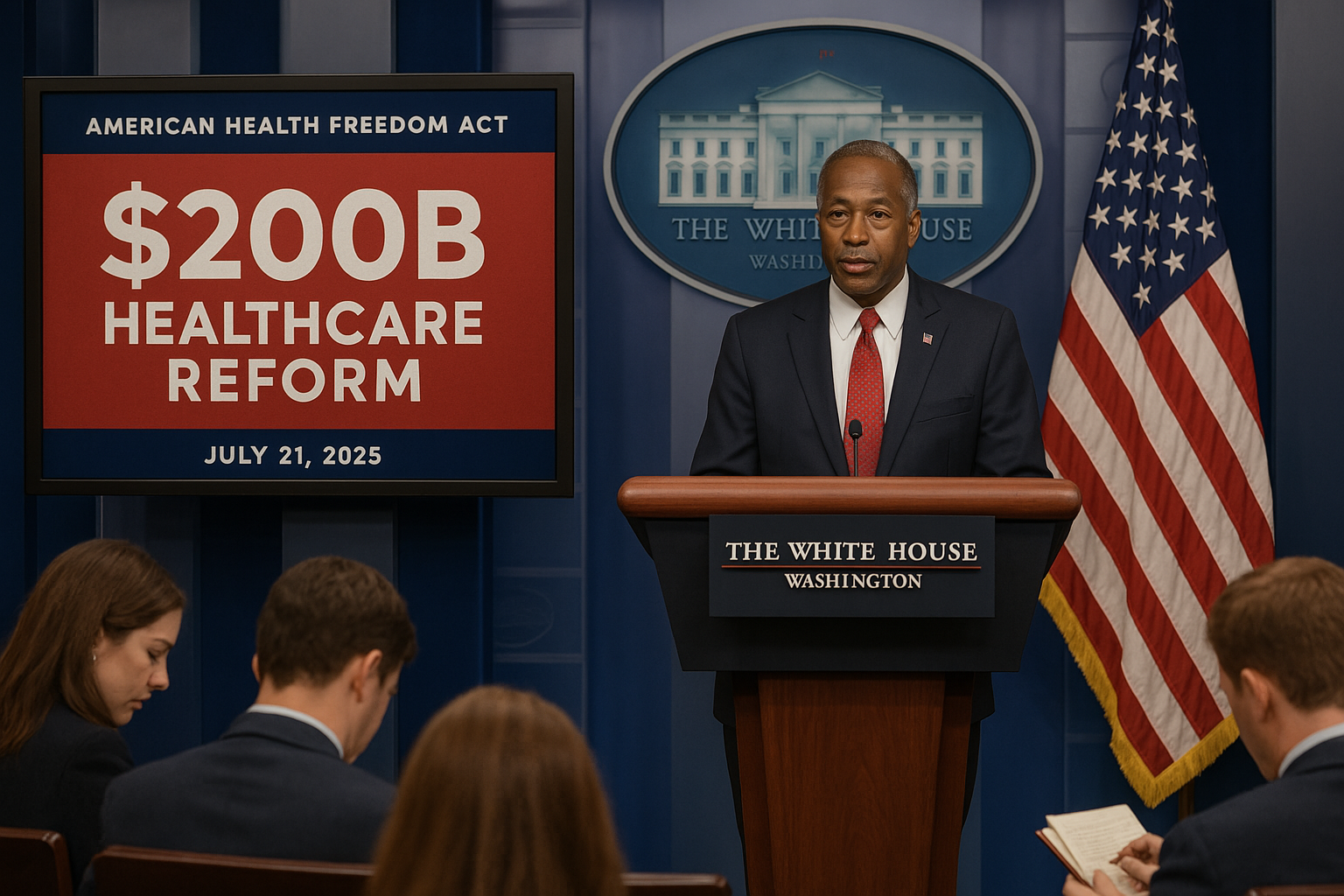
On July 21, 2025, the Trump administration unveiled a sweeping $200 billion healthcare reform plan in Washington, D.C., aimed at overhauling the Affordable Care Act (ACA) and addressing rising costs exacerbated by recent tariffs. Announced by Health and Human Services Secretary Dr. Ben Carson at a White House press briefing, the “American Health Freedom Act” promises to expand access through tax credits, deregulate insurance markets, and incentivise private-sector innovation. The proposal, set to be debated in Congress next month, responds to growing public demand for affordable healthcare as inflation, driven by a 1% rise in household goods prices, squeezes families.
Reform Details
The plan allocates $120 billion for tax credits to low-income families, $50 billion for rural hospital modernisation, and $30 billion for AI-driven telemedicine platforms. It replaces ACA mandates with flexible state-run exchanges, allowing insurers to offer low-cost, high-deductible plans. Carson emphasized reducing bureaucracy, citing a 15% administrative cost reduction goal. The proposal also includes price transparency rules, requiring hospitals to publish service costs online, and a $10 billion fund for opioid crisis treatment, addressing a 20% rise in overdoses in 2024, per CDC data.
The reform leverages technology, with partnerships like Nexus Innovations in Indianapolis developing AI diagnostics to cut costs by 10%. However, it faces opposition from Democrats, who argue it weakens protections for pre-existing conditions. The announcement, covered by NBC News, trended on X, with @HealthCareNow praising the rural focus but warning of coverage gaps, gaining 15,000 views.
Context and Implications
Healthcare costs have surged, with tariffs increasing medical equipment prices by 5%, per Reuters. The CPI rose 2.7% in June, driven by tariff-sensitive goods, adding pressure on families. The reform aligns with national trends, like Chicago’s airline merger, where consolidation aims to offset economic pressures. By decentralizing insurance, the plan mirrors New York’s fintech deregulation, fostering competition but risking uneven access, as only 60% of rural Americans have broadband for telemedicine, per FCC data.
The proposal responds to public frustration, with 70% of Americans citing healthcare costs as a top concern, per a Gallup poll. It also reflects Trump’s push for deregulation, seen in the EPA’s research unit closure, prioritizing market-driven solutions over federal oversight.
Community and Fan Response
D.C. residents rallied outside the Capitol, with supporters chanting “Freedom in Health!” while critics, including AARP, warned of premium hikes for seniors. On X, @DCPolicyWatch noted 18,000 views, debating the plan’s impact on Medicare. The National Urban League urged equitable access, noting that 25% of Black Americans lack adequate coverage. Community groups in rural Ohio, a key reform target, are planning forums to discuss the plan, expecting a 10% boost in local healthcare jobs.
Challenges and Opportunities
The reform faces a divided Congress, with House Speaker Mike Johnson securing a 219-213 vote for tax cuts but struggling with healthcare consensus. Implementation challenges include state capacity to manage exchanges, with only 20 states fully prepared, per the Kaiser Family Foundation. Tariff-driven cost increases could offset savings, as seen in a 1.9% appliance price surge. Opportunities lie in AI adoption, potentially reducing diagnostic errors by 15%, and rural investments, which could add 5,000 hospital beds by 2030.
Economic and Social Impact
The plan is projected to save $50 billion annually by 2028, per CBO estimates, but risks leaving 5 million uninsured if states opt out, per Urban Institute. Economically, it could stimulate healthcare tech, adding $20 billion to GDP, similar to California’s solar boom. Socially, it aims to empower underserved communities, but disparities persist, with 30% of Hispanic Americans uninsured, per Census data. Community clinics in Texas are expanding to offset gaps, mirroring flood recovery efforts.
Future Outlook
The reform’s fate hinges on Senate approval, with a vote expected by September. Success could reshape healthcare, positioning the U.S. as a leader in market-driven systems, like New Jersey’s fintech hubs. Failure risks deepening public distrust, with 65% of voters demanding action, per Pew Research. The administration plans to pilot programs in Indiana and Florida by 2026, leveraging local sports enthusiasm to promote wellness campaigns.
Conclusion
The American Health Freedom Act is a bold bid to redefine U.S. healthcare, balancing innovation with risks of inequity. As Congress debates, its outcome will shape the nation’s economic and social fabric, echoing transformative efforts in other sectors.